The Truth About the Menstrual Cycle
Most women are misinformed and it's not their fault
It’s absurd how misinformed most women are about their menstrual cycle. But it is not these women’s fault. Accurate information about how the female body works can be surprisingly hard to find. In my opinion, the crux of this confusion is the very misleading representation of how exactly our hormone levels fluctuate throughout the menstrual cycle, as presented by most medical/biology textbooks, online fertility articles, and books written by “fertility specialists” alike. A correct understanding of how exactly our hormonal levels change throughout the menstrual cycle, and how these changes affect us physically and mentally, is crucial to ensuring good health and quality of life. Research shows that nearly 50% of reproductive-age women worldwide deal with PMS (premenstrual syndrome). I expect this figure to be even higher since many women have been conditioned to accept unacceptable symptoms as normal.
PMS has multifaceted and often hellish manifestations. Symptoms such as painful breasts, digestive disturbances, nausea, migraines, acne and water retention and the exacerbation of autoimmune conditions, epilepsy, mood disorders, anxiety, allergic reactions, eating disorders and substance abuse are only some of the symptoms that many women are faced with in the week (or two) before their menstrual bleed. Women suffering from PMS tend to feel their worst after ovulation, in the luteal phase, which is the latter half of their cycle. In a woman with a regular, ovulatory, 28-day cycle, the luteal phase should last two weeks, starting just after ovulation (which often happens on day 14 of the cycle, but not always), and ending around day 28, just before the onset of the menstrual bleed. This is the time when hormonally-driven negative symptoms are amplified.
Some women experience symptoms so severe that I have more than once heard the phrase “Women are meant to feel well only one week per month.” For most women, this “good” week happens during the follicular phase, the first half of their cycle. PMS symptoms are classic signs of estrogen excess, yet women are told that estrogen is highest in the first half of their cycle when they feel their best. This contradiction puzzled me until I realized that misleading data and poor research practices have led women (and certain health authorities) to accept the following (incorrect) assertions as fact:
The follicular phase (the first half of the menstrual cycle) is a phase of high estrogen
The luteal phase (the second half of the menstrual cycle) is a phase of low estrogen
Increased progesterone in the luteal phase is what causes PMS
Again, this is incorrect, and I will provide data to support this. I find this information to be insanely important to bring awareness to, as whether it is you, the reader, suffering from PMS, or whether you have a girlfriend, sister or friend suffering from it, PMS often fails to be properly addressed. The lack of less invasive treatment options for PMS (largely due to misunderstandings about its etiology) leads many women to hysterectomies/oophorectomies (the surgical removal of the uterus and/or ovaries to stop the menstrual cycle entirely) or hormonal contraceptives (which act akin to chemical castration by fully suppressing the ovaries’ ability to release hormones). To solve the problem, we must first correctly identify it.
THE FOLLICULAR PHASE IS NOT A HIGH ESTROGEN PHASE
Many health publications, such as the one below, claim that PMS is caused by declining estrogen levels after ovulation. However, this isn’t true:
“Changes in hormone levels are thought to be the main cause of PMS/PMT. More specifically, it is the decline in oestrogen and rise in progesterone for up to two weeks before the period starts.”
— The Surrey Park Clinic
I believe every woman has seen the menstrual cycle graph that looks something like the above, that comes from a respectable medical journal publication. The common menstrual cycle graph shows estrogen levels being high in the follicular phase, peaking at ovulation, and decreasing after ovulation while progesterone rises. This is only partly true. While progesterone levels should rise exponentially after ovulation, estrogen levels do not decrease; they stay elevated or can increase further. Data shows that, across a regular, 28-day ovulatory cycle, estrogen levels can be 6x higher in the luteal phase than in the follicular phase. This is why symptoms of estrogen dominance are more pronounced in the luteal phase (the latter half of the cycle).
DATA SUPPORTING HIGH ESTROGEN LEVELS IN THE LUTEAL PHASE
One 2005 study of female cyclists with regular menstrual cycles, in their early to mid-twenties, found their estrogen levels to be:
Up to 264 picomoles per litre in the early follicular phase
Up to 1328 picomoles per litre at ovulation & during the luteal phase
The study looked at both trained and untrained female cyclists, measuring their sex hormones during the early follicular phase, ovulation (late follicular), and mid-luteal phase. In the study, “late follicular” refers to ovulation, meaning that from ovulation onwards, women tend to have higher levels of estrogen. Some of the participants in the untrained sample had higher estrogen levels in the luteal phase than at any other point in their cycle, including ovulation, which is colloquially taught to women as the time in their cycle when their estrogen levels should be the highest. In the untrained sample, the highest estrogen concentration observed in the luteal phase was 1613 picomoles per liter, while the highest estrogen concentration at ovulation observed was 1118 picomoles per liter. If we graph the average recorded estrogen levels and the highest recorded estrogen levels for each part of the cycle in this study (for the combined trained and untrained groups), this is what the graphs end up looking like:
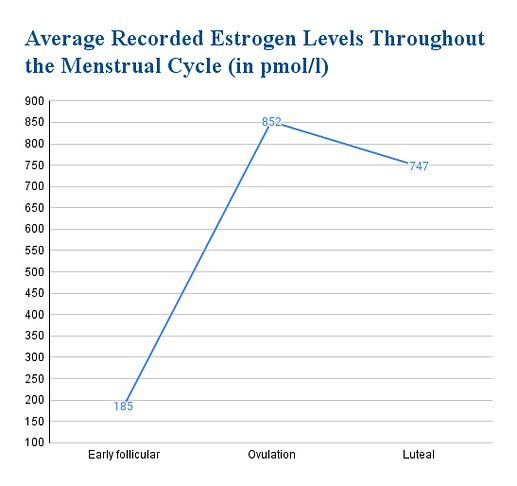

This is in stark contrast to the graphs found in fertility textbooks and publications alike which show estrogen being high in the follicular phase and dropping in the luteal phase. Another study of 12 women with healthy cycles found that estrogen levels ranged from 83.3 pmol/l to 171 pmol/l in the follicular phase, and from 341.3 to 1040.3 pmol/l in the mid-luteal phase, a nearly tenfold increase in estrogen for some women.

Yet another study tracking 60 women with self-reported healthy, regular menstrual cycles for two months found similar results, with estrogen levels higher in the luteal phase than in the follicular phase. The measurements were taken during week 1 of the cycle and again 8 days after a positive ovulation test.
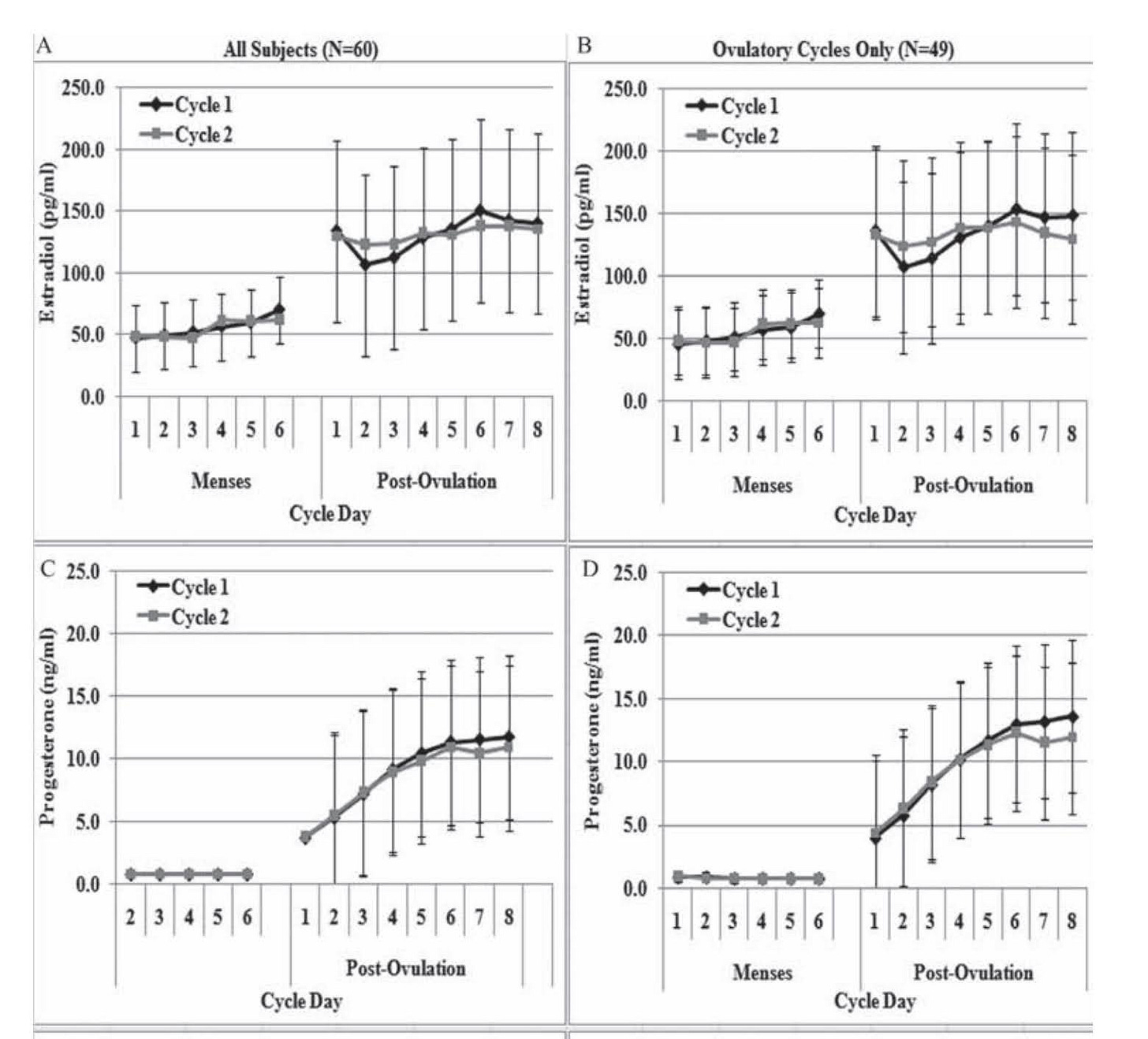
These findings contrast with traditional menstrual cycle graphs, which show estrogen being high in the follicular phase and dropping in the luteal phase. Yet, schools still teach girls that it’s the follicular phase that’s a phase of high estrogen, leaving them confused and wondering why their symptoms of estrogen dominance happen later in their cycle.
A more accurate graph would show both estrogen and progesterone being low in the follicular phase and high in the luteal phase.
With estrogen concentrations being so much higher in the luteal phase, estrogen dominance is more pronounced in the luteal phase, and this is what causes women to suffer.
PROGESTERONE TAKES THE BLAME FOR WHAT ESTROGEN DOES
Since progesterone levels rise exponentially in the luteal phase (or, at least, they should), many have been led to believe that progesterone is the “bad guy,” and the cause behind PMS. However, bio-identical progesterone has successfully treated PMS many times. Dr. Katharina Dalton, a pioneer in PMS research, demonstrated in her work that PMS is brought on by a deficiency of progesterone or a deficiency relative to estrogen. Her body of work (including multiple books) documents hundreds of cases of women getting relief from PMS after being administered bio-identical progesterone. In one of her earlier published papers, of 61 women suffering from PMS who received progesterone injections, 83.5% became symptom-free. Ideally, the elevated progesterone levels during the luteal phase should protect against deleterious high estrogen levels, since, although both adequate estrogen and progesterone levels are needed for a healthy menstrual cycle, they are like yin and yang. Progesterone acts in ways that are largely opposite to the functions of estrogen, guiding and restraining estrogen’s actions. When the two are imbalanced, estrogen can become destructive. Estrogens cause tissue proliferation, while progesterone mostly causes differentiation. Estrogen causes tissues to retain water, while progesterone acts as a diuretic. Estrogen can contribute to mental disturbances by increasing the release of cortisol by the adrenal glands and slowing the breakdown of adrenaline. Progesterone, on the other hand, lowers cortisol levels and attenuates the activation of the HPA axis. Estrogen increases glutaminergic activity in the brain, the excess of which can result in nervous symptoms such as nail biting, OCD, body dysmorphia, and ADHD. Progesterone increases GABA, which opposes the excitatory effect of glutamate. Estrogen promotes the release of histamine. Progesterone inhibits histamine secretion.
Poor dietary habits, such as skipping meals, fasting, eating salads as meal replacements, low carb diets and avoiding animal foods, can lower active thyroid hormone levels, needed to release progesterone and support the liver in clearing excess estrogen.
However, producing enough progesterone in the luteal phase, making sure that this progesterone can bind to its receptors, being able to prevent the over-production of estrogen and ensuring adequate clearance of it by the liver, gut and kidneys, are all dependent on the body having adequate cellular energy. The production and utilization of this energy are dependent in part on a nutrient-dense diet, adequate in calories, carbohydrates, animal protein, minerals, and fat and water-soluble vitamins. Poor dietary habits, such as skipping meals, fasting, eating salads as meal replacements, low carb diets and avoiding animal foods, can lower active thyroid hormone levels, needed to release progesterone and support the liver in clearing excess estrogen. Animal protein (including glycine, found in gelatin), dietary carbohydrates and nutrients like vitamins E, B6, C, and zinc are needed to produce progesterone and clear excess estrogen. In an undernourished body, PMS thrives. Dr. Dalton discovered that eating a starch-containing meal every 3-4 hours alleviated PMS completely in 19% of participants without needing supplemental progesterone. Progesterone can’t exhibit its protective actions when blood sugar falls too low. “Progesterone receptors do not bind to molecules of progesterone in the presence of adrenalin, which is released when the blood glucose level is low. While awaiting their first appointment, 84 women with severe premenstrual syndrome (PMS) completed a questionnaire detailing all food and drink consumed on seven consecutive days. The average daytime interval between starch-containing foods was 7 hours, with an overnight interval averaging 13 ½ hours. This suggested that women with PMS might benefit from shorter food intervals between starch-containing foods and avoidance of large meals. On receipt of their questionnaires women were advised to follow a three-hourly starch diet, which was beneficial in 54 per cent with improvement in a further 20 per cent. The diet alone proved effective in 19 per cent, who needed no additional medication for full relief of premenstrual symptoms.” Many women under-eat, skip meals, and avoid animal protein and dietary sugars. Combined with exposure to environmental xenoestrogens, phytoestrogens from foods like soy, and polyunsaturated fats (which interfere with the liver’s ability to detoxify old estrogens), the imbalance between progesterone and estrogen in the luteal phase becomes greater, resulting in often agonizing symptoms.
LUTEAL PHASE DIETARY SUPPORT
Apart from eating enough and eating often, consider incorporating the following foods in your diet to increase progesterone and balance estrogen levels for a smooth luteal phase.
RIPE FRUIT
Carbohydrates, especially from ripe fruit (with ample potassium and vitamin C), lower cortisol and adrenaline while increasing thyroid hormone levels, helping us use progesterone. Citrus fruits, like oranges, contain flavonoids, such as naringin, which lower the excessive production of estrogen by body fat stores.
OYSTERS
High in magnesium and zinc, which help regulate pituitary gland activity, necessary for ovulation and progesterone production. Selenium and iodine in oysters help to make thyroid hormones.
LIVER
High in vitamin A, vitamin E, copper, and B vitamins, all essential for progesterone production.
BUTTER
Butter is a rich source of cholesterol, a primary building block of all hormones. Butter is one of the only foods naturally high in progesterone. One study found that of all dairy products, butter has the highest progesterone concentration, at 130-300 ng/g.
RAW CARROTS & WELL-COOKED VEGETABLES
Fiber helps excrete old estrogens and toxins and prevents re-absorption.
SCALLOPS
Rich in taurine, supporting liver function to eliminate excess estrogen.
I hope this article clarifies why symptoms of estrogen dominance flare up in the luteal phase and reinforces that progesterone is not the villain in this battle.
Poor research practices have contributed to the misunderstanding of progesterone’s role in PMS. Low levels of allopregnanolone (a direct metabolite of progesterone), are a known feature of PMS. Yet, failing to take into consideration the absorption rate of certain routes of administration of progesterone and mixing data from studies using bioidentical progesterone with those using synthetic progestins, which only partially resemble progesterone’s action, while having more in common with the estrogens and androgens, has muddied the findings on the role of progesterone in the treatment of PMS, and estrogen in causing it.
This article was written by Kaya. You can reach her on Instagram @fundamental.nourishment. If you enjoyed the read, consider checking our her Substack publication, Fundamental Nourishment. She writes about topics such as metabolic health, estrogen dominance, and other fertility myths we have been taught. Subscribe here:
This article was originally published in Issue 27 of the WARKITCHEN Magazine. Access the rest of our magazines and all of our links here. Godspeed 🥂
Kaya’s other articles dive deeper into topics such as metabolic health, estrogen dominance, and other fertility myths we have been taught. Some of them may be of interest:
Content for entertainment purposes only. Not medical or health advice.















And this is how we take the control back over our bodies 🤝🏼
Obsessed with this piece, especially about foods for luteal support. Full of gems. I learned about all of these things wayyy too late in life, and wish I’d known so much sooner— thank you for writing this. 🫐